12 Common Public Health Issues and How They Can Be Prevented

Tables of Contents

What’s the goal of public health? Quite simply, it’s to protect and improve the well-being of individuals and communities. How? By fighting disease and promoting healthy lifestyles. Public health addresses chronic conditions and emergency health threats ranging from heart disease and depression to infectious diseases and violent injuries.
Public health workers are vital to safeguarding a population’s health. These individuals investigate, monitor, prevent, and treat health conditions that impact society. They conduct tasks such as disease research and response, community education and outreach, and injury prevention to meet specific health-related goals.
Public health programs vary in scope. A community-based program might seek to improve diabetes care services in a town experiencing high rates of obesity, while a state or national public health program might focus on a mental health condition disproportionately impacting a certain demographic group.
The need for robust public health programs and trained health professionals becomes evident when considering the scope and scale of these common public health issues:
- Cardiovascular disease
- Type 2 diabetes
- Hypertension
- Schizoaffective disorder
- Clinical depression
- Borderline personality disorders
- Opioid addiction
- CNS depressant abuse
- Prescription stimulant abuse
- Panic disorder
- Social anxiety
- Phobias
Truncal Obesity Issues: The Wide Impact They Have on Health
The prevalence of obesity in the U.S. population is skyrocketing, jumping from about 30% in 2000 to more than 40% in 2018, according to the U.S. Centers for Disease Control and Prevention (CDC). Obesity contributes to numerous health conditions, including heart disease, diabetes, stroke, and cancer.
More than half of obese individuals store excess fat around the abdomen, according to the ACSM’s Health & Fitness Journal article “Targeting Abdominal Obesity Through Diet.” Truncal obesity, or abdominal obesity, is considered extremely harmful due to the proximity of vital organs to fatty tissue in the truncal area.
Abdominal obesity is related to environmental conditions, such as diet and exercise, and genetic factors. Rates of abdominal obesity are higher in women and older adults.
A community health program looking to lower obesity rates might work to:
- Educate residents about healthy eating
- Improve access to healthy foods
- Facilitate access to affordable healthcare resources
Meanwhile, a state public health agency might investigate rates of obesity among different ethnic groups to discover why cases are higher among certain populations, exploring factors such as income levels, living situations, and crime rates.
Public Health Issue #1: Cardiovascular Disease
Cardiovascular diseases — primarily heart disease and stroke — are the leading global cause of death, according to the World Health Organization (WHO). Common heart diseases include coronary artery disease, arrhythmia, and cerebrovascular disease.
Health factors that contribute to heart disease include:
- High blood pressure
- Elevated glucose levels
- Raised lipid levels
The concentration of fat in the truncal area is connected to the buildup of plaque in arteries, which creates increased risks for cardiovascular disease. One recent study found that heart attack patients with abdominal obesity were more likely to have recurring atherosclerotic cardiovascular disease.
The instance of heart disease in obese patients can be addressed through public health programs that aim to improve diet and exercise habits and promote weight loss. These programs educate community members on risks such as:
- Dangers of eating energy-dense foods with high fat and sugar contents
- Health impacts of physical inactivity
- Cardiovascular risks related to smoking
Public health programs may also identify high-risk members of the community. They connect these clients with healthcare resources, including treatment, medication, and counseling.
Public Health Issue #2: Type 2 Diabetes
Diabetes is another top cause of death worldwide. The condition occurs when the pancreas doesn’t produce enough insulin (Type 1 diabetes) or when the body cannot process insulin (Type 2 diabetes).
Of the 34 million U.S. residents with diabetes, more than 90% have Type 2 diabetes, according to the CDC. One in five diabetes patients don’t know they have the disease.
Over time, diabetes may cause damage to the:
- Heart
- Eyes
- Kidneys
- Nerves
- Blood vessels
Abdominal obesity is connected to a number of metabolic disorders including insulin sensitivity and glucose intolerance, two key factors in the development of diabetes. Obesity can also increase the risk of complications from diabetes such as diabetic neuropathy.
In addition to advising populations on the benefits of consuming nutrient-rich foods and getting regular exercise, public health programs can help reduce instances of diabetes and diabetes-related conditions through regular health screenings. Early diagnosis is key to preventing and treating diabetes.
Public Health Issue #3: Hypertension
Another symptom of obesity is hypertension, or high blood pressure, which is a key contributor to heart disease. Screenings for high blood pressure are part of routine preventive care protocols.
However, some populations don’t have proper access to routine medical care or can’t afford care services. Millions of adults have uncontrolled hypertension, which can be managed with diet, exercise, and medication.
When conducting obesity prevention programs, public health officials:
- Collect research on health trends in communities and demographic groups
- Monitor the outcomes of specific intervention programs to determine which efforts are most effective
- Share data to form best practices, and develop training programs and support resources for partnering groups
National and global organizations, such as the CDC and WHO, act as catalysts for improving population health outcomes.
Truncal Obesity Resource Guide
The following articles and websites provide insight on abdominal obesity and related recurring health conditions:
Abdominal Obesity and Metabolic Syndrome: Exercise as Medicine?: A review of metabolic syndrome and how it may be treated with exercise from BMC Sports Science, Medicine and Rehabilitation
Diabetes: Facts on diabetes and how to prevent the disease from the CDC
Experimental Weight Gain Increases Ambulatory Blood Pressure: A study showing the relationship between obesity and hypertension from Mayo Clinic
High Blood Pressure Symptoms and Causes: Statistics and facts on hypertension from the CDC
Obesity and Overweight: Statistics and facts on obesity from the World Health Organization
The Health Risks of Abdominal Obesity: Definition and risks of truncal obesity from Verywell Health
The Link Between Abdominal Fat and Repeat Heart Attacks: A summary of research on abdominal fat and cardiovascular conditions from Medical News Today
2020 Topics & Objectives: Heart Disease and Stroke: Risk factors and preventive measures for cardiovascular conditions from the U.S. Office of Disease Prevention and Health Promotion
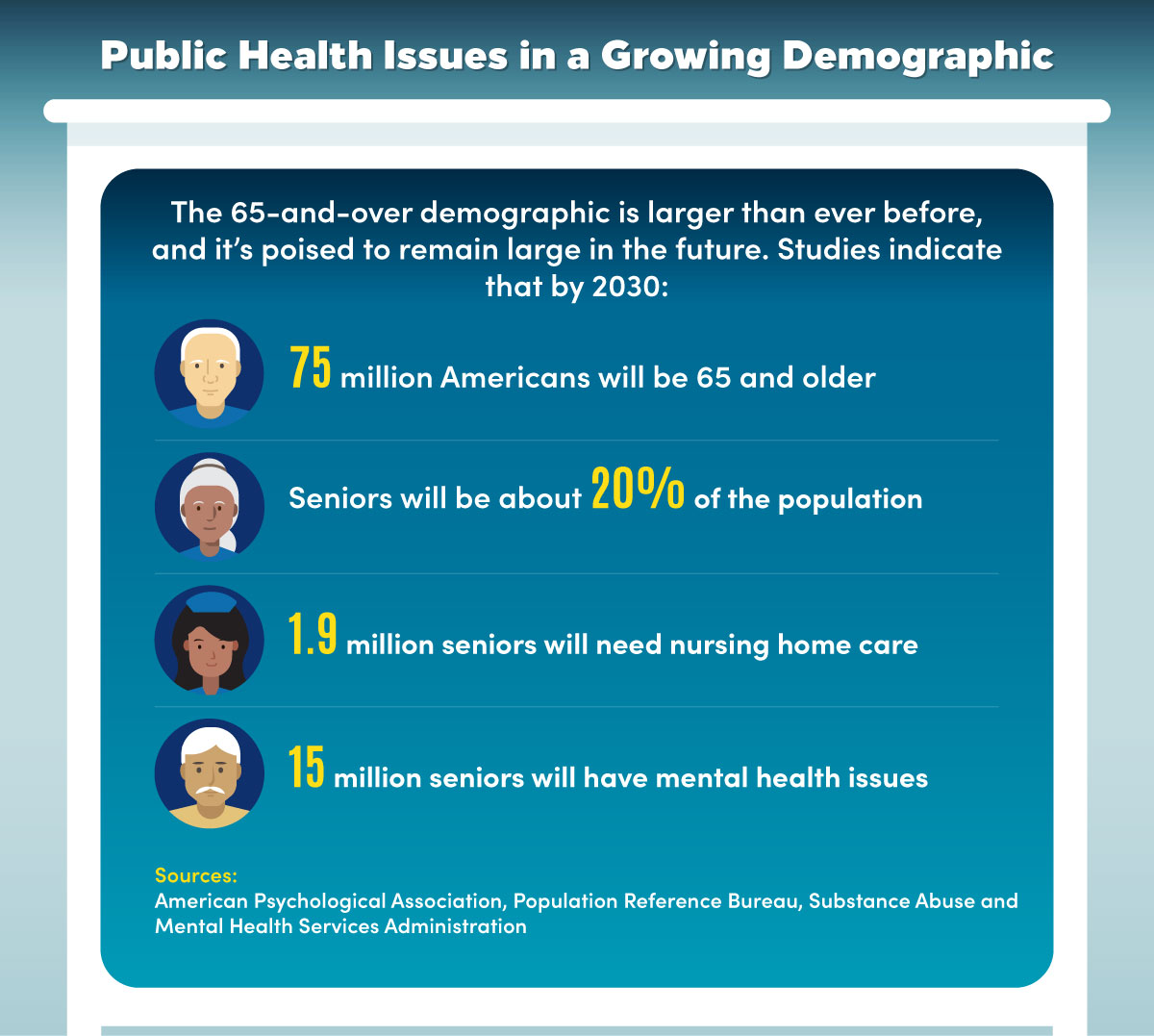
Senior Mental Health and Public Health Response
The senior population in the U.S. is growing rapidly, with the portion of residents age 65 and older expected to increase from 17% to 20% of the population between 2020 and 2030, according to the latest population projections from the Census Bureau.
The increasing number of seniors is straining public health systems in the U.S. and other nations around the globe.
Senior citizens are experiencing rising rates of conditions including:
- Obesity
- Economic disparity
- Isolation
- Alzheimer’s disease
This results in an increased demand for nursing home care and other services.
The aging population is also experiencing rising rates of mental illness. An estimated 1 out of 5 older adults has a mental health condition or substance abuse disorder, according to the Substance Abuse and Mental Health Services Administration (SAMHSA).
Public Health Issue #4: Schizoaffective Disorder
Schizoaffective disorder is characterized by symptoms of both schizophrenia (such as delusions or hallucinations) and mood disorders (such as depression or mania). The condition is also marked by disorganized thinking and depressed mood.
The condition can be caused by:
- Stress
- Genetics
- Brain chemistry
Public health organizations looking to address senior mental health issues such as schizoaffective disorder will typically work to connect seniors with counseling services, including teletherapy (virtual counseling), and psychiatrists who can prescribe helpful medications.
Public Health Issue #5: Clinical Depression
Clinical depression is a serious chronic mental health ailment. Symptoms of depression include loss of appetite, lack of energy, restlessness, and loss of interest in activities. When left untreated, depression can lead to illness, fatigue, and even suicide.
Many seniors are isolated in their homes or living in nursing homes. This can make it difficult to identify serious mental health concerns. Late-life depression impacts some 6 million seniors in the U.S., according to WebMD.
Instances of late-life depression are higher among:
- Women
- Single individuals
- People without a social network
- Individuals who have experienced stressful events
Medical conditions such as hypertension, diabetes, dementia, chronic pain, and cancer can also increase depression risk.
Public health workers can help educate seniors, nursing home operators, medical professionals, and other community members on the signs of depression in older adults. Public health programs might also conduct mobile screenings at senior centers to identify at-risk individuals.
Public Health Issue #6: Borderline Personality Disorders
Borderline personality disorder (BPD) is a mental health condition characterized by difficulty managing emotions and behavior. Individuals with the condition typically have:
- Self-image issues
- Concerns of abandonment
- Impulsive behaviors
- Intense emotional reactions to stress
- Patterns of unstable relationships
In addition to BPD, other types of personality disorders include paranoid personality disorder and antisocial personality disorder. Personality disorders often manifest in adults, and can worsen or improve with age. Personality disorders in seniors might be characterized by irrational thoughts or actions, or abrupt changes in mood.
Making sure that seniors have access to diagnostic and treatment resources is essential to public health programs. Many public health agencies are incorporating mental health goals into their chronic disease prevention efforts. These goals include:
- Conducting research on the prevalence of mental health conditions such as BPD among population groups
- Identifying and eliminating risk factors and disparities
- Raising awareness of mental health issues
- Increasing access to mental health treatment programs
Senior Mental Health Resource Guide
The following articles and websites provide insight on senior care and mental health conditions:
Aging in the United States: Fact sheet on the aging population from the Population Reference Bureau
Assessing an Older Adult’s Mental Health Needs: Guidelines on how to identify mental health issues in older adults from AARP
Behavioral Health: Information and intervention tips for seniors facing mental health concerns from the National Council on Aging
Borderline Personality Disorder: Information on symptoms and causes of borderline personality disorder from Mayo Clinic
Bringing Awareness to the Mental Health of Older Adults: Statistics on the instance of mental health conditions among older Americans from SAMHSA
Depression in the Elderly: Information on how depression can be identified and treated in elderly populations from WebMD
Older Adults’ Health: Advocacy resources for applying psychology to improve health in older adults from the the American Psychological Association
Signs of Prescription Drug Abuse
Drug overdose deaths have risen sharply in the U.S., with more than 750,000 people dying from drug overdoses between 1999 and 2018, according to the CDC. Many of those deaths were caused by prescription drug abuse, in addition to illegal drug use. The rate of overdose deaths was four times higher in 2018 than in 1999.
Signs of prescription drug abuse, according to addiction and substance abuse resources from the American Psychiatric Association, include:
- Taking larger amounts of drugs than prescribed
- Experiencing an inability to cut back on drug use
- Expending great effort obtaining drugs, such as visiting multiple doctors
- Finding difficulty in fulfilling work, school, or home obligations
- Exhibiting reduced activity levels
- Struggling with social or interpersonal problems
- Experiencing drug withdrawal symptoms
Older adults are more likely to accidentally misuse or abuse prescriptions. That’s because they often manage multiple prescriptions for chronic conditions, which can cause adverse drug interactions, according to the U.S. National Institute on Drug Abuse. Older adults also have a slower metabolism, which affects how quickly the body breaks down drugs.
Public Health Issue #7: The Opioid Crisis
Opioid abuse is the largest contributor to drug overdose deaths. Much of the current opioid crisis is due to the overprescribing of common prescription painkillers such as hydrocodone (Vicodin) and oxycodone (OxyContin or Percocet).
Other types of opioids that contribute to the epidemic are heroin and synthetic opioids (fentanyl and tramadol, either prescribed or manufactured illegally).
Some of the effects of opioids include:
- Euphoria
- Confusion
- Drowsiness
- Nausea
According to the CDC, opioids account for about 70% of overdose deaths, with two-thirds of deaths caused by synthetic opioids and nearly one-third from common prescription painkillers.
In the U.S., federal and state governments have launched extensive public health programs to combat the epidemic. Steps include:
- Educating physicians on proper opioid prescribing practices
- Updating opioid prescription tracking systems
- Improving fatal and nonfatal drug overdose tracking systems
- Supplying emergency responders with overdose treatments
- Enhancing access to care for people with drug use disorders, including through community health clinics
Public Health Issue #8: CNS Depressant Abuse
Central nervous system depressants, or sedatives, are prescribed for conditions such as anxiety, panic attacks, sleep disorders, or tension. CNS depressants include benzodiazepines (Valium, Librium, and Xanax) and barbiturates (Mebaral and Nembutal).
When sedatives are taken in large doses, they can cause:
- Slowed reflexes
- Impaired thinking
- Blurred vision
- Slurred speech
Overdoses can result in unconsciousness, coma states, or death. Per the National Institute on Drug Abuse, some 10,700 overdose deaths from benzodiazepines were recorded in 2018 (out of about 67,400 total overdose deaths). Many of these deaths involved the combined use of benzodiazepines and opioids.
Public health programs increase access to recovery services. This can include identifying those with sedative abuse disorders and connecting them to health resources including addiction rehabilitation centers.
Treatments include supervised detoxification, counseling, and behavioral therapy. These public health programs might target high-risk communities, such as low-income urban neighborhoods or rural towns with insufficient health resources.
Public Health Issue #9: Prescription Stimulant Abuse
Prescription stimulants are medications that are typically prescribed to people with conditions such as attention deficit hyperactivity disorder (ADHD) or narcolepsy. These drugs increase attention, energy, and alertness.
Common prescription stimulants include:
- Dextroamphetamine (Dexedrine)
- Dextroamphetamine and amphetamine combinations (Adderall)
- Methylphenidate (Ritalin and Concerta)
Psychostimulants with abuse potential, including prescription stimulants and illicit drugs such as methamphetamine, accounted for 12,700 overdose deaths in 2018, according to the National Institute on Drug Abuse. This number has risen each year since 2014, with and without involvement of other substances.
Substance abuse disorders can lead to other public health problems, according to the U.S. Office of Disease Prevention and Health Promotion, such as:
- Domestic violence
- Motor vehicle accidents
- Crime
- Suicide
- Teenage pregnancy
- Child abuse
Public health interventions might target at-risk adolescents, working with schools to deter drug use in youth through education campaigns.
Prescription Drug Abuse Resource Guide
The following articles and websites provide insight on instances and signs of prescription drug abuse:
Opioid Overdose: Statistics and public health initiatives for drug abuse prevention from the CDC
Overdose Death Rates: Data on overdose deaths by drug classification from the U.S. National Institute on Drug Abuse
Prescription Drug Overdose: Resources on drug abuse public health efforts from the American Public Health Association
Prescription Opioids: Information on opioids and abuse factors from the U.S. National Institute on Drug Abuse
Prescription Stimulants: Information on psychostimulants from the U.S. National Institute on Drug Abuse
Sedatives: Symptoms and causes of CNS depressant use from Psychology Today
2020 Topics & Objectives: Substance Abuse: Information on substance abuse risks and interventions from the U.S. Office of Disease Prevention and Health Promotion
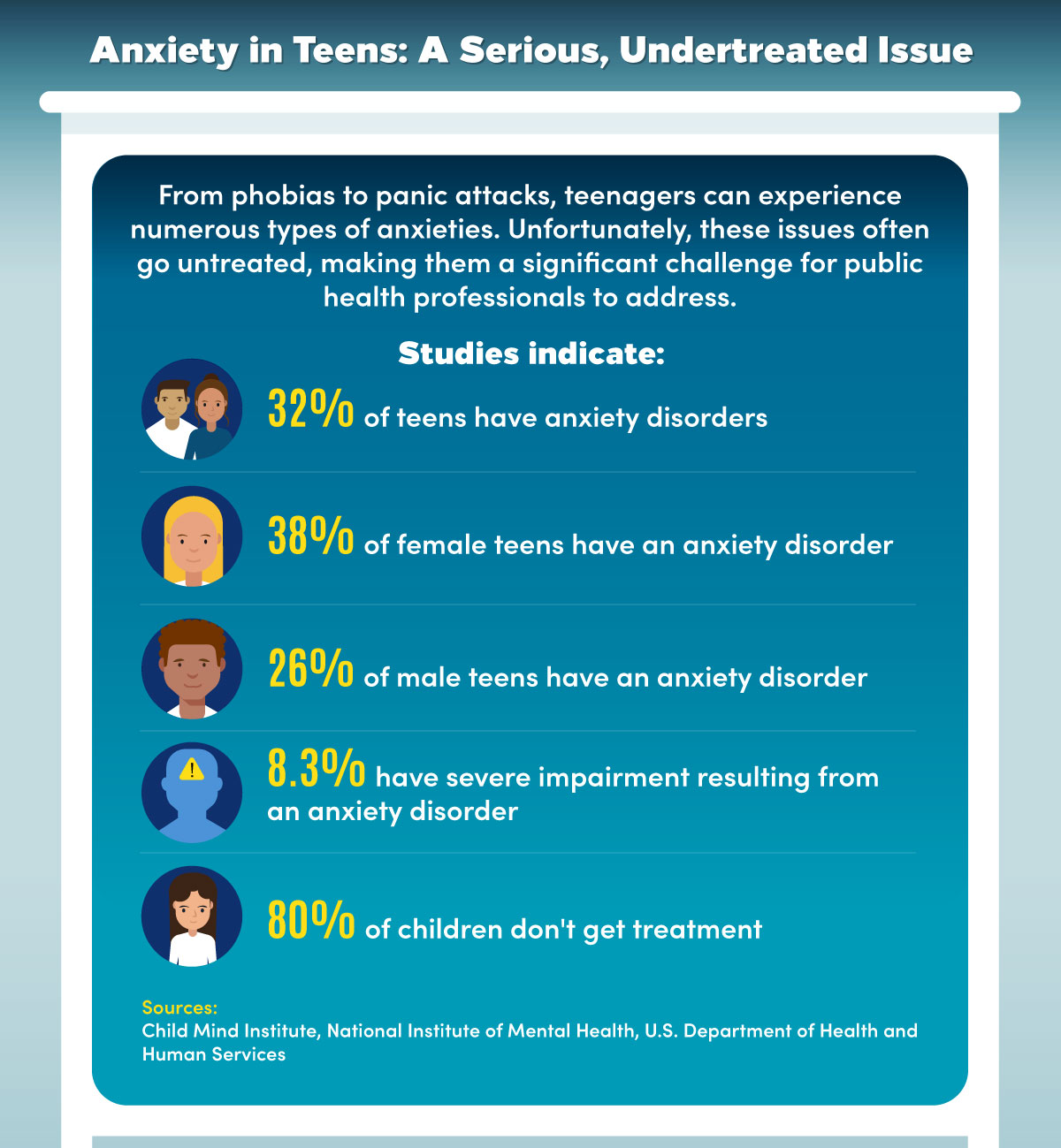
Teenage Anxiety: Issues and Treatments
Anxiety is one of the most common mental health disorders. Among youth, some 7.1% of children between the ages of 3 and 17 have been diagnosed with anxiety, according to the CDC. Anxiety in children often occurs with other conditions, such as depression or behavioral problems. Anxiety can present itself as fear or shyness.
Symptoms of anxiety include:
- Sudden episodes of intense fear
- Constant worry about things that might happen
- Extreme fear of a specific object or place
Some of the physical symptoms of anxiety include:
- Trouble sleeping or concentrating
- Dizziness and shaking
- Sweating
- Increased heart rate
- Irritability and anger
- Headaches and stomach ailments
- Muscle tension
Anxieties can manifest in adolescence and intensify during the teenage years. If left undiagnosed or untreated, anxiety can interfere with school attendance, work performance, and family relationships.
Public Health Issue #10: Panic Disorder
Panic disorders are characterized by sudden, unexpected bouts of intense fear. Teens with panic disorders typically experience panic attacks that last several minutes and cause dizziness, increased heart rate, and difficulty breathing.
Treatment measures include cognitive behavioral therapy — where counselors help individuals examine their thoughts around anxiety-producing activities — and medications such as antidepressants.
Public health programs seeking to address teenage anxiety conditions such as panic disorder may seek to improve mental health parity, or equal insurance coverage and access to mental health services. Public health workers might also seek to improve community awareness and prevention efforts for related problems such as suicide and gun violence.
Public Health Issue #11: Social Anxiety
Social anxiety is an extreme fear of social situations such as attending parties or giving speeches in class. Teens with social anxiety may fear being humiliated or judged by peers. These individuals may struggle to form friendships and have high rates of school absences or poor grades.
Causes of anxiety conditions such as social anxiety include:
- Family history of anxiety
- Brain chemistry or personality
- Traumatic experiences such as violence or death of loved ones
- Child abuse
- Drug or alcohol use
- Family divorce or separation
- Poverty
To address teenage anxiety, public health workers might seek to increase awareness of crisis hotlines, peer support groups, and counseling resources. They might also work with schools to improve access to on-campus or virtual counseling services. Connecting teens with preventive healthcare services and conducting mental health screenings are also key.
Public Health Issue #12: Phobias
Phobias range from a fear of spiders to anxiety induced by small spaces. People with phobias typically avoid triggering objects or situations. They may experience intense fear or panic attacks when encountering triggers.
Symptoms of phobias often start during childhood, with the average onset age of 7, according to the Anxiety and Depression Association of America (ADAA).
Types of phobias include:
- Agoraphobia (fear of certain situations or places)
- Fear of flying or driving
- Emetophobia (fear of vomiting)
- Health anxieties
Cognitive behavioral therapy and exposure therapy — the guided effort to confront fear-inducing activities — can be effective methods of treating phobias. Family therapy can work to improve communication skills and help build support resources in the home. In addition to therapy and medication, teens can use some self-treatment techniques to curb the effects of phobias.
Some examples of these techniques include:
- Meditation or yoga
- Exercise
- Deep breathing
- Relaxation training
- Self-help books
Teenage Anxiety Resource Guide
The following articles and websites provide insight on teenage anxiety and related conditions:
Anxiety and Depression in Children: Data on signs and treatments for child mental health conditions from the CDC
Anxiety Disorders: Symptoms and treatment information from Mayo Clinic
Best Medications for Kids With Anxiety: Information on prescription treatments for anxiety from the Child Mind Institute
Data and Statistics on Children’s Mental Health: Data on instances of mental health conditions in children from the CDC
Facts and Statistics: Data on anxiety rates and risk factors from the ADAA
How to Deal with Anxiety: Tips on anxiety treatments from Crisis Text Line
Public Health Addresses Population Needs
Public health programs seek to address major public health issues such as depression, anxiety, drug abuse, and obesity. Health agencies need to be flexible to address the needs of vulnerable communities, which can change when new economic, social, or population health issues arise.
For instance, when a pandemic outbreak occurs, public health workers may provide needed disease testing, contact tracing, or patient support services. Public health programs might also need to adapt to conditions such as an increase in domestic violence or higher rates of asthma among community residents.
These programs can make a huge difference in the quality of life for at-risk populations. Public health’s goal is to enhance the well-being of individuals and communities, and public health workers play a vital role in improving population health outcomes.

