Physician Burnout by Specialty: What It Is and How to Avoid It
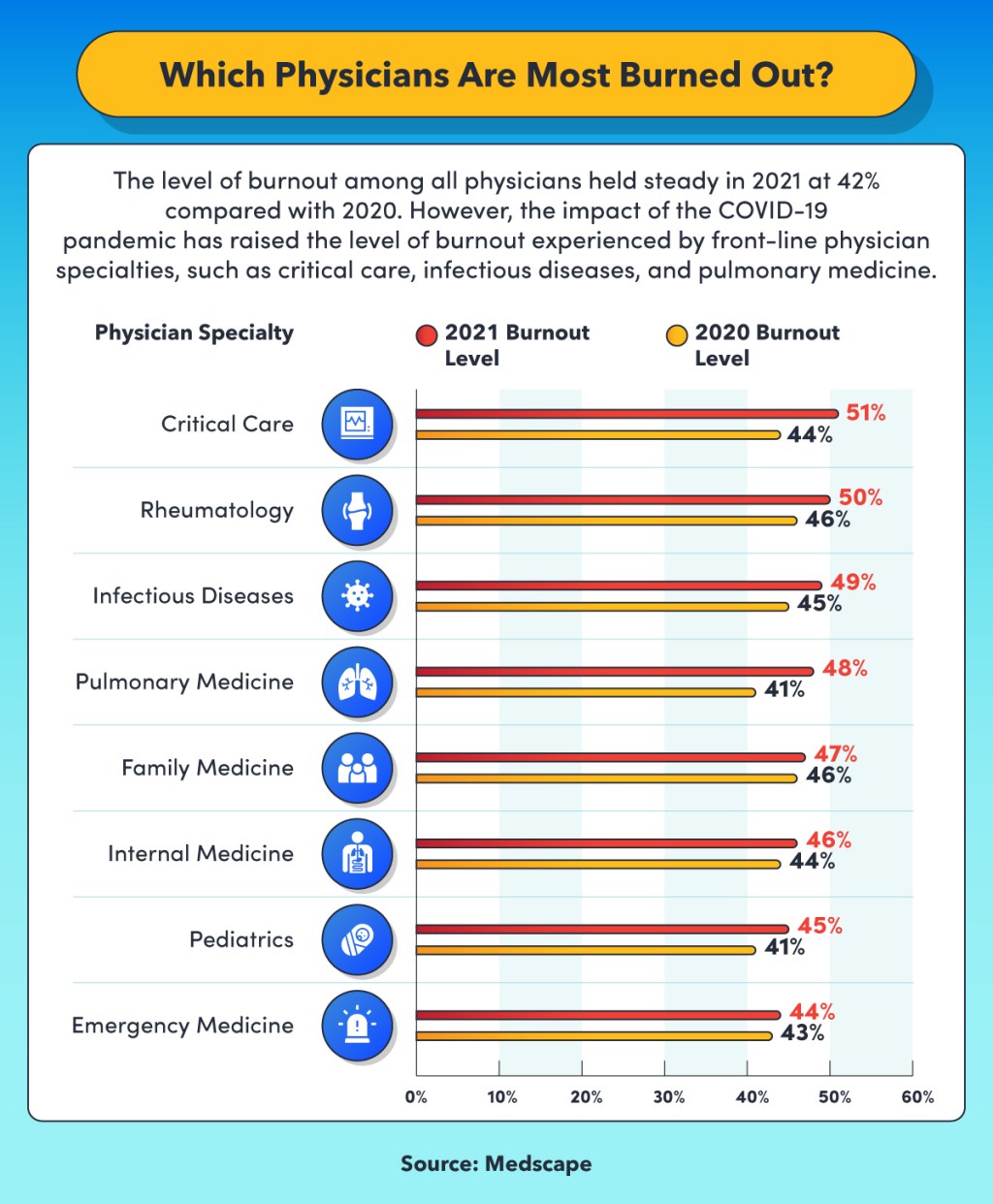
Table of Contents
The primary reason most physicians enter the profession is a desire to help people in need. However, with each passing year, physicians in all specialties spend less time interacting with their patients and more time dealing with administrative duties. The result is unprecedented levels of physician burnout.
- A 2021 Medscape survey of physician burnout and suicide found that 42% of all physicians felt burned out.
- A 2020 Medical Economics survey found that 91% of doctors experienced burnout related to their work at some time in their careers, and 71% said they felt burned out at the time of the survey.
- According to the Medical Economics survey, the main causes of physician burnout are too much paperwork and regulations (cited by 31% of physicians), poor work-life balance/long working hours (15%), and the COVID-19 pandemic (12%).
Physician burnout affects the healthcare industry by reducing the quality of care and hindering patient outcomes. The problem also exacerbates the critical shortage of physicians by discouraging qualified candidates from entering the profession. While burnout impacts certain physician specialties more than others, all areas of medicine become more susceptible to burnout in the aftermath of disasters, such as the COVID-19 pandemic, and in other stress-inducing circumstances.
By examining physician burnout by specialty, effective approaches can be devised to identify its causes and develop strategies to avoid and treat the problem.
Physician burnout broken down by specialty
The pressures that the COVID-19 pandemic has placed on healthcare systems worldwide illuminate the economic, social, and political forces that threaten the ability of physicians and other healthcare professionals to provide adequate service to their patients. Macroeconomics is the “primary driver of burnout,” according to a healthcare leader quoted by the American Medical Association (AMA).
- Economic inequality and social justice issues affect the culture in hospitals and other healthcare institutions across the U.S.
- At the organization level, administrative burdens and operational inefficiencies that exacerbate economic disparities and social injustice drive physician burnout.
- At the personal level, physicians struggle to balance their work lives with their family obligations and personal needs.
While burnout affects all areas of medicine to some extent, the rate of burnout is higher among certain specialties. Medscape’s survey noted a change in stress levels resulting from the COVID-19 pandemic.
- In the 2021 Medscape survey, the specialties reporting the highest levels of physician burnout were critical care, rheumatology, and infectious diseases.
- This is a shift from the 2020 Medscape survey, where the specialties reporting the highest levels of burnout were urology, neurology, nephrology, endocrinology, and family medicine.
The Medscape survey also found that physician burnout varies only slightly by work setting.
- Healthcare organizations: 47%
- Outpatient clinics: 46%
- Office-based multispecialty group practice: 44%
- Nonhospital academic, research, government, or military: 42%
- Hospital: 40%
- Office-based single-specialty group practice: 40%
- Office-based solo practice: 40%
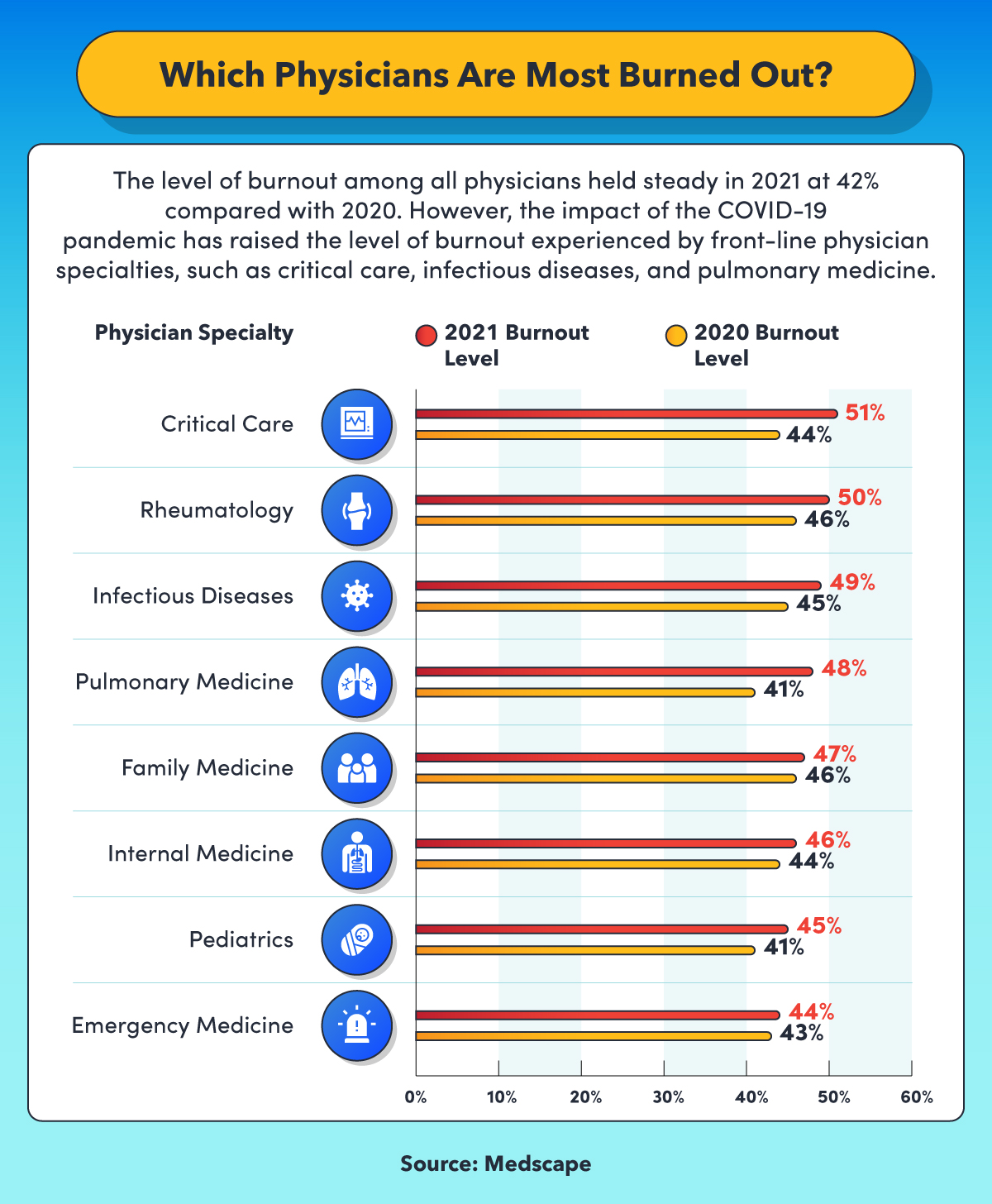
The level of burnout among all physicians held steady in 2021 at 42% compared to the previous year, according to Medscape. However, the impact of the COVID-19 pandemic has raised the level of burnout experienced by front-line physician specialties, such as critical care, infectious diseases, and pulmonary medicine. Critical care: 51% burnout level in 2021, 44% in 2020. Rheumatology: 50% in 2021, 46% 50% in 2020. Infectious diseases: 49% in 2021, 45% in 2020. Pulmonary medicine: 48% in 2021, 41% in 2020. Family medicine: 47% in 2021, 46% in 2020. Internal medicine: 46% in 2021, 44% in 2020. Pediatrics: 45% in 2021, 41% in 2020. Emergency medicine: 44% in 2021, 43% in 2020.
The impact of stressful events on physician burnout rates
Stressful events, such as natural disasters and pandemics, may lead to a surge in physician burnout for those practicing in specific areas. Responding to the massive influx of patients with COVID-19 put great pressure on healthcare systems and workers as they dealt with shortages of personal protective equipment (PPE), long working hours, grieving families, and other difficult working conditions.
However, when physicians were asked in the Medscape survey when they first felt symptoms of burnout, 79% said before the COVID-19 pandemic, and just 21% said after the pandemic’s start. An American Society of Clinical Oncology (ASCO) study reports that the pandemic increased the level of stress and burnout that oncologists experienced.
- Fear of exposure to COVID-19 caused personal and familial stress among the oncologists interviewed.
- Many of the oncologists were concerned that the pandemic would disrupt patient care, interrupt education and research efforts, and hurt the financial health of their practice.
- Several of the physicians considered retiring early or working part time.
Physicians and other healthcare professionals on the front line of the fight against the pandemic feel the impact most. The New York Times cites a critical care physician in Missouri who reported that caseloads at his hospital increased by 40% in two weeks in June 2021. An emergency room doctor whose work covers parts of South Dakota and Wyoming worried that the high number of people refusing vaccinations in his practice area threatened the health of his children.
Common causes of physician burnout among medical specialties
A significant factor in preventing physician burnout is being able to integrate work life with personal life. A study of work-life integration among U.S. physicians published in the Journal of the American Medical Association (JAMA) found that when compared with internal medicine subspecialties, four physician specialties reported a much lower level of work-life integration:
- Urology
- Emergency medicine
- General surgery
- Neurosurgery
The study determined that the physicians who reported the lowest work-life integration scores were single women aged 35 and older who worked long hours and had more call nights per week.
Even though working as a physician is inherently stressful, certain conditions and characteristics of the profession contribute to burnout:
- Nonclinical burdens, such as billing, insurance, documentation, and workplace politics
- Inefficient electronic health records (EHRs) and lack of administrative support
- Loss of autonomy and control
- Inflexibility in work environments
- Deteriorating patient-physician relationships, possibly causing a loss of meaning in the work
What is physician burnout?
Defining what physician burnout is combines the general characteristics of burnout — exhaustion, alienation from work activities, reduced performance — with the challenges and responsibilities of treating people with acute, chronic, and life-threatening injuries and diseases. Research published in Local and Regional Anesthesia reports that symptoms of burnout are more prevalent in physicians than in the general population: 37.9% of physicians vs. 27.8% of all professions.
The characteristics of specific physician specialties make them more prone to causing burnout. Specialties on the front line of care are at greater risk, including family medicine, general internal medicine, and emergency medicine. These areas of care are subjected to more of the internal and external factors that contribute to burnout in physicians:
- External factors include demanding work; time pressures; contradictory instructions; lack of freedom to make decisions; lack of organizational influence; poor internal communication; pressure from superiors; increasing responsibilities; poor teamwork; problematic rules and policies; and a lack of staffing, funding, and other resources.
- Internal factors include high self-expectations that border on idealism, perfectionism, the need for recognition, a drive to please others, suppressing their own needs, thinking of themselves as irreplaceable, overestimating their ability to overcome challenges, substituting their work for their social life, and failing to seek meaningful activities outside of work.
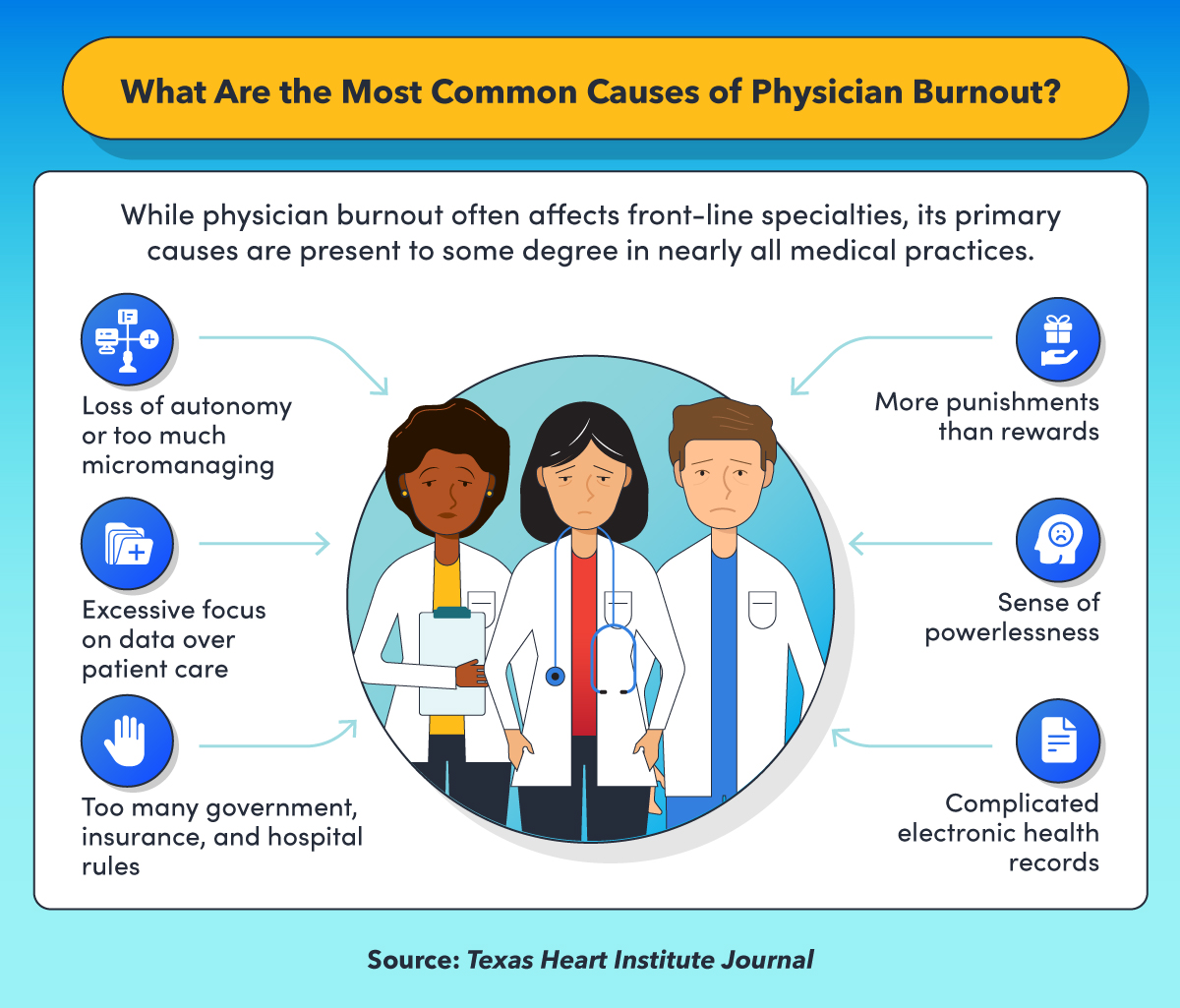
While physician burnout often affects front-line specialties, its primary causes are present to some degree in nearly all medical practices. According to the Texas Heart Institute Journal, these causes include: loss of autonomy or too much micromanaging; excessive focus on data over patient care; too many government, insurance, and hospital rules; more punishments than rewards; sense of powerlessness; and complicated electronic health records.
Physician burnout definition
Physician burnout is a self-reported condition characterized by feelings of emotional exhaustion and depersonalization. The symptoms of physician burnout include irritability, detachment, and failure to recognize personal accomplishments. The World Health Organization (WHO) classifies burnout as an occupational phenomenon rather than a medical condition.
- It results from a failure to manage chronic workplace stress.
- It causes feelings of energy depletion and exhaustion.
- It leads to physicians taking a negative and cynical view of their work and profession.
- It makes physicians less effective in their work.
One definition of physician burnout is that it’s a long-term stress reaction causing depersonalization, cynical and negative attitudes toward patients, a lack of empathy, and feelings of failure or career disappointment. Rather than occurring all at once, burnout develops in five stages, as described in the Local and Regional Anesthesia report:
- The honeymoon phase is characterized by enthusiasm.
- At the onset of excessive stress, stagnation sets in as work becomes the physician’s sole focus at the expense of family, social life, and personal priorities.
- Over time, the physician begins to experience chronic stress, which leads to feelings of frustration, a perception of failure, and a sense of powerlessness.
- Physicians begin to believe that their efforts are wasted and that they’re not sufficiently recognized, causing apathy, despair, and disillusionment.
- Finally, physicians come to feel trapped, which leads to habitual burnout and a sense of resignation and indifference toward their work.
At the final stage, physicians feel mentally, physically, and emotionally exhausted to the point that they need to seek help and intervention. By this time, they’ve often lost their commitment to patients and coworkers, and their cognitive performance has declined, along with their motivation, creativity, and judgment. All aspects of their lives suffer, possibly leading to chronic sadness and depression.
Resources on physician burnout by specialty
- National Institute for Health Care Management, Physician Burnout & Moral Injury: The Hidden Health Care Crisis — The infographic presents a range of statistics relating to physician burnout, including the physician specialties that are most susceptible to the condition.
- Association of American Medical Colleges, Well-Being in Academic Medicine — Dozens of links to articles and other resources that describe how to recognize and prevent burnout in medical faculty members, clinicians, researchers, residents, and others involved in academic medicine.
Physician burnout statistics by specialty
Stress affects physicians at all stages of their careers, from medical school and residency to board certification in a specialty to well into their work lives. Physician burnout statistics illustrate the pervasiveness of the condition and the challenges in addressing the problem.
- A study reported in JAMA found that medical school students who experience mistreatment and have an unfavorable perception of the learning environment are more likely to experience high levels of exhaustion and disengagement, lower levels of empathy, and career regret than students who have a positive medical school experience.
- AMA’s research during the COVID-19 pandemic found that 27% of physician residents experienced high levels of stress, 53.47% of which they attributed to fear of exposure to the virus. In addition, 30% of residents said they felt anxious and overworked during the pandemic, and 50.5% had symptoms of burnout.
- Growing shortages in physician specialties contribute to burnout and poor patient outcomes. The Association of American Medical Colleges (AAMC) forecasts that demand for surgical specialists will exceed supply by between 17,100 and 28,700 surgeons by 2033. The projected shortage of all nonprimary care specialty physicians is between 33,700 and 86,700 by 2033.
Physician burnout is more prevalent among intensive care unit (ICU) and other critical care physicians, and research suggests that burnout among critical care physicians leads to more errors and compromises patient safety.
How various practice areas are affected by physician burnout
The workload and stress of treating patients with severe COVID-19 symptoms have wreaked havoc on one physician specialty in particular: ICU and other critical care physicians. Scientific American reports on a recent survey that found that more than half of all critical care physicians felt burned out. Among the factors contributing to the high level of burnout among this physician specialty are:
- Shortage of PPE
- 5% mortality rate of COVID patients admitted to ICUs
- Concerns for their personal safety
- Feeling unable to provide patients with the emotional support they need
Burnout is prevalent in many physician specialties outside of critical care. A recent survey of rheumatology physicians found that 50.8% felt at least one of the three Maslach Burnout Index (MBI) measures: emotional exhaustion, depersonalization, and lack of personal accomplishment. A primary factor contributing to burnout among rheumatology specialists is dissatisfaction with EHRs, especially their usability and the time the record keeping takes away from time spent with patients. The study indicates that physicians who spend more than 20% of their time performing meaningful activities are less likely to experience burnout.
A survey of internal medicine physicians at hospitals in British Columbia sought to measure the prevalence of physician burnout during the pandemic. The study concluded that 68% of all the physicians surveyed had MBI symptoms of burnout. Specialties with the highest prevalence of burnout were respirologists, infectious disease physicians, oncologists, nephrologists, and physicians working in social medicine.
Resources providing physician burnout statistics
- Golden Source Consultants, Clinical Wellness Survey Resources for 2021 — Statistics and resources on the impact of physician burnout on the likelihood of malpractice and on the quality of care patients receive.
- Frontiers in Public Health, “Prioritizing the Mental Health and Well-Being of Healthcare Workers: An Urgent Global Public Health Priority” — A survey of research on burnout among physicians and other healthcare workers before and during the COVID-19 pandemic.
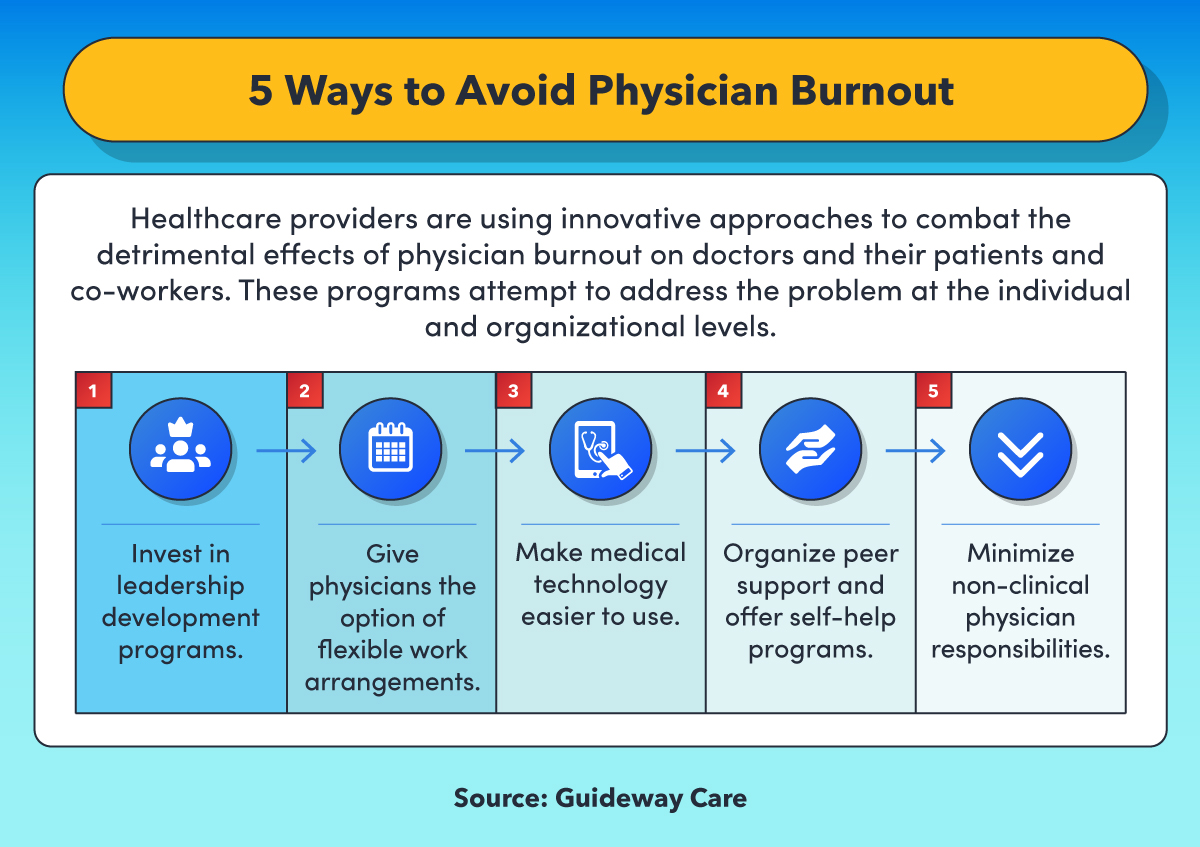
Healthcare providers are using innovative approaches to combat the detrimental effects of physician burnout on doctors and their patients and coworkers. According to Guideway Care, these programs attempt to address the problem at the individual and organizational levels: invest in leadership development programs; give physicians the option of flexible work arrangements; make medical technology easier to use; organize peer support and offer self-help programs; and minimize non-clinical physician responsibilities.
Physician burnout treatment methods
Treating physician burnout faces two big obstacles: the reluctance of physicians to ask for help and to accept treatment. A 2020 American College of Emergency Physicians (ACEP) poll found that while 87% of emergency room physicians reported feeling more stress and 72% stated they were experiencing more burnout, 45% of the physicians were reluctant to seek mental health treatment. In addition, 73% believed that a stigma is attached to seeking mental health treatment.
Physicians hold themselves to a high standard for resilience and the ability to handle stress. They value their professional identity and reputation for putting their patients’ interests first. Evidence-based strategies to reduce physician burnout look for solutions to the problem in terms of workload, job demands, lack of control, work flexibility, and work-life integration.
The AMA offers four approaches to reducing physicians’ workloads, work schedules, and time demands:
- Standardize: The most efficient way to run a healthcare operation is by making layouts, offices, and equipment arrangements as close to identical as possible. This reduces the amount of time physicians have to spend thinking about where things are as they move from area to area.
- Eliminate redundancies: The processes that physicians rely on for completing records, submitting orders, and receiving information should be performed consistently. For example, lab results that are delivered by text may not need to be sent by email as well.
- Automate EHRs: The medical data that physicians need to enter into EHRs should be consolidated and presented in a way that makes all necessary information accessible in a single location.
- Reduce interruptions: All members of the physician’s medical team need to understand what conditions warrant an interruption. Physicians should be allowed to block out some time with no interruptions to complete necessary tasks that require their full attention.
Helping physicians balance work and personal lives
Physicians are expected to be “able, affable, and available,” but Medical News Today points out that of the three, available is often the easiest of the three to achieve. The 24/7/365 nature of a physician’s potential schedule makes it challenging to maintain a regular life outside of work. Establishing a clear and consistent separation between a physician’s work and personal life requires finding a purpose, managing time, prioritizing, and reassessing.
- Purpose: As often as possible, physicians should take part in the activities that remind them why they became doctors, such as taking time to connect with patients and motivating them to take steps to improve their health.
- Time management: Physicians should always have short- and long-term goals in mind, make plans, and avoid activities that take up too much of their time. They can create templates for EHRs, avoid technology disruptions, and use mobile devices to complete paperwork while in transit.
- Priorities: Many workdays in physicians’ lives can feel like nonstop triage, but they need to always stay focused on the most important thing at each moment; often it’s not what others believe is most important. They need to filter out the many distractions that prevent attention being spent on what needs to be done right now.
- Reassessment: Some life transitions are planned, and others are unexpected, but both types are opportunities to reconsider goals and plans and reset when necessary. A physician’s work-life balance is always in motion and often requires work adjustments.
Programs to help physicians overcome work-related stress
Physicians need to recognize the symptoms of professional burnout and know when to seek assistance. Among the approaches used to help physicians avoid burnout and maintain a healthy perspective about their work are peer-to-peer programs, programs that physicians participate in before their stress levels reach burnout levels, and programs that connect physicians with mental health resources outside of their own organization.
- Peer-to-peer programs: The AMA reports that being able to connect with other physicians offers a nonjudgmental environment free of stigma and typically outside of the processes of the physician’s own institution. Discussing burnout with a peer helps physicians validate their emotions and experiences and understand that what they’re feeling is normal.
- Pre-burnout stress management programs: Routine mental health screening provides physicians with an opportunity to gauge their own stress levels. Screenings make it easier for physicians to find out about burnout-reducing resources available to them.
- Outside programs: The Physician Well-Being and Burnout Initiative from the American Psychiatric Association (APA) offers interventions for physician burnout that serve the needs of individuals and organizations. It also provides links to online resources for physicians with depression and addictions.
Resources for identifying and overcoming physician burnout
- National Academy of Medicine, Action Collaborative on Clinician Well-Being and Resilience — A program intended to raise awareness of burnout, anxiety, and depression among physicians and other healthcare professionals and to improve patient care by “caring for caregivers.”
- AMN Healthcare, “The Mental Health Impacts of Healthcare Burnout” — A white paper proposing a new approach to mental health among physicians, nurses, and other healthcare workers that emphasizes mindfulness and meditation.
Improving healthcare by helping physicians avoid and overcome burnout
Communities rely on physicians of all specialties for their well-being. The continuing shortage of physicians means that women and men in the profession may need to work more efficiently and effectively to meet the growing demand for their valuable services. Recognizing and treating the signs of physician burnout is healthy for physicians, their patients, and their communities.
Infographic Sources
Guideway Care, “Reducing Physician Burnout: 5 Strategies”
Medscape, “‘Death by 1000 Cuts’: Medscape National Physician Burnout & Suicide Report 2021”
Medscape, “Medscape National Physician Burnout & Suicide Report 2020: The Generational Divide”
Texas Heart Institute Journal, “Physician Burnout: Causes, Consequences, and (?) Cures”

