Healthcare Management Terms for High School Students

Tables of Contents

Healthcare management professionals are critical members of the healthcare community with a wide range of responsibilities, including implementing technologies that improve patient care, managing budgets for healthcare facilities, and ensuring that healthcare laws are followed. An understanding of healthcare terms is essential for every aspect of a healthcare management professional’s role.
From drug delivery and billing to insurance claims and outpatient services, a clear understanding of healthcare terms — and the important health policies connected to certain terms — enables healthcare management professionals to help ensure effective, efficient patient care delivery. On the other hand, when these healthcare concepts are unclear, it can pose health risks to patients and increase healthcare costs.
Healthcare managers ensure clear communication in healthcare settings and use their knowledge of healthcare terms and policies to help patients:
- Know their healthcare options
- Avoid misunderstandings and understand the care they’re receiving
- Understand healthcare insurance terminology, which can make the process of working with their insurance companies a bit easier
- Overcome barriers to healthcare access
Students who plan to pursue healthcare careers should get an early start in familiarizing themselves with key healthcare terms. In this article, we will define and examine the importance of concepts including:
- Health Insurance Portability and Accountability Act (HIPAA)
- Pre-existing conditions
- Acute illness
- Anti-inflammatory medication
What Does HIPAA Stand for, and Why Is It Important?
One important term that healthcare professionals use is HIPAA compliance. HIPAA, which stands for Health Insurance Portability and Accountability Act, plays a vital role in protecting patient security and safety. HIPAA is important because it establishes standards and rules for protecting sensitive patient data. At the same time, it provides guidance on the proper sharing of patient information.
For example, when a healthcare manager shares patient information with clinicians in another practice caring for the same patient, they must comply with HIPAA regulations by ensuring that only the information necessary for proper patient care is shared, and that the data is transmitted in a safe manner. Using their knowledge of HIPAA, healthcare management professionals can help safeguard against misuse of patient data while communicating information that leads to higher quality care.
Essential HIPAA requirements deal with disclosure of patient data; interoperability of systems shared between providers; digitization of data; security involved in sharing data; and protecting electronic health records (EHRs) from unauthorized access, alteration, and deletion.
Keeping patient data safe is an important part of HIPAA privacy regulations. However, the law allows flexibility in terms of who can access patient data and when. For example, hospitals typically maintain facility directories, or databases of current patients’ names, overall health conditions, and locations in the facility. A hospital can disclose directory information about a patient to anyone who asks for the individual by name, provided the patient gives informal consent. However, patients are sometimes incapacitated and unable to give consent. In this case, HIPAA permits healthcare facilities to exercise their judgment about which information can be shared if it’s in the best interest of the patient.
One of the challenges of HIPAA compliance in healthcare data revolves around a misunderstanding about the rules. For instance, clinicians may fail to share important information with a consulting physician due to concerns over not having proper consent. However, a healthcare manager with a firm understanding of HIPAA rules can help determine when it’s proper to disclose information. This knowledge will help ensure the practice is meeting HIPAA regulations, avoiding penalties and legal action.
Another challenge derives from a failure to implement the technology to support HIPAA compliance. HealthITSecurity reports that 51% of healthcare providers fall short of compliance with HIPAA right of access rules. The regulation promotes the sharing of medical information with patients in digital format. However, the form and format of medical records often preferred by patients don’t conform to the digital standard. “Eighty-six percent of non-compliant providers were out of compliance for this reason,” according to the report. As technology implementation is a critical component of the healthcare manager role, it’s imperative that an aspiring healthcare manager understand the technology requirements set forth by HIPAA regulations.
Making changes to healthcare facility operations to meet HIPAA requirements can be costly to healthcare providers. They can also face fines and penalties for failing to meet HIPAA rules. Knowledgeable healthcare managers can share information, implement processes, conduct audits, and deliver compliance training to healthcare staff to ensure that HIPAA rules are followed.
HIPAA resources and additional information
- The American Academy of Pediatrics (AAP) addresses decades-long misperceptions about the HIPAA Privacy Rule and provides answers to frequently asked questions.
- In its Data Insider blog, Digital Guardian provides insights into the role information security plays in HIPAA compliance.
- For information on the HIPAA Privacy Rule and Security Rule, the U.S. Department of Health and Human Services (HHS) provides a summary, which includes descriptions of key definitions used in the regulation. HHS.gov also offers a resource that provides answers to commonly asked questions about facility directories as they pertain to HIPAA rules.
What Is a Pre-existing Condition?
A Kaiser Family Foundation report cites that almost 54 million people in the U.S. have a pre-existing health condition. The term pre-existing condition defines an illness or health condition that a patient was known to have before signing up for health insurance. Were it not for the Affordable Care Act (ACA), individuals with pre-existing health conditions would continue to only have limited access to health insurance coverage options.
Before the passage of the ACA, people with conditions ranging from minor (for example, tonsillitis and menstrual irregularities) to major (for example, AIDS/HIV, cancer, diabetes, and dementia) could have trouble gaining health insurance coverage. Private insurers in the individual plan market could deny or charge more for coverage, while employer plans could impose waiting periods for coverage of pre-existing conditions. The current rules that made it illegal for insurance companies to deny people health coverage due to a pre-existing condition went into effect on January 1, 2014. Only grandfathered individual health insurance policies, those that started on or before March 23, 2010, weren’t subject to ACA rules. For individuals with pre-existing conditions enrolled in these plans, it means that a healthcare insurer could either cancel their policy or increase their premiums.
Patients with pre-existing conditions often pay out-of-pocket expenses for healthcare services. Aspiring healthcare managers should understand common terms used for out-of-pocket expenses, including the following:
- Deductible. A deductible is the flat fee that patients are responsible for before insurance companies pay for healthcare services. For example, if a deductible is $1,000 a year, the insurance will only pay for medical services after a patient has paid $1,000 in healthcare service costs.
- Copayment. A copayment is a fixed fee that patients pay for a medical service covered by an insurance company. It’s typically paid in advance at a medical appointment. The healthcare provider charges the patient’s insurance company for the remaining cost of the medical services provided.
Trends suggest rising out-of-pocket costs for people with insurance plans. For example, according to a report from the Peterson Center on Healthcare and the Kaiser Family Foundation, about a decade ago, only 59% of people with employer-sponsored healthcare plans had deductibles to pay at medical appointments. The number has risen dramatically to 85% as of May 2019.
Still, were it not for the ACA, patients with pre-existing conditions would see even higher out-of-pocket costs. According to a report from The Commonwealth Fund, “Average out-of-pocket costs for those with cancer or diabetes would triple, while costs for arthritis, asthma, and hypertension care would rise by 27% to 39%.”
Additional information about pre-existing conditions
- HealthCare.gov provides information on 10 essential health benefits covered by marketplace health insurance plans under ACA rules.
- HHS.gov and Investopedia explain what pre-existing conditions are and offer additional insights.
- Policygenius provides a list of common pre-existing conditions that were typically denied coverage before ACA.
Acute and Chronic Illnesses: Differences and Examples
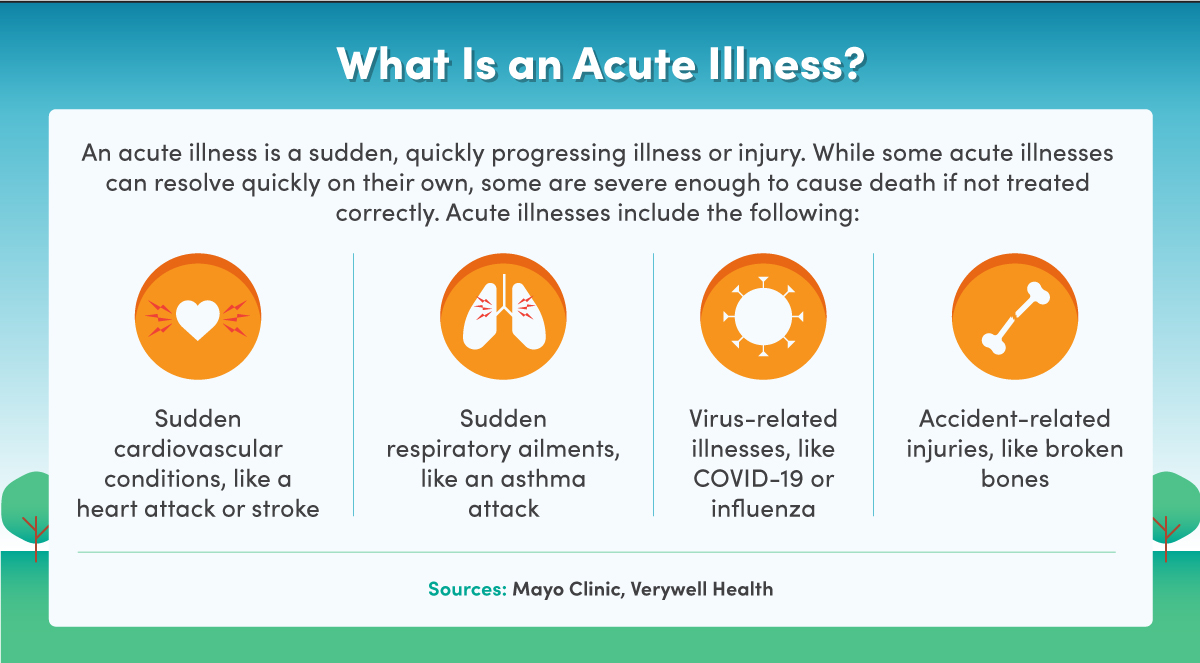
Pre-existing conditions are typically chronic diseases, such as diabetes, hypertension, and cancer. Acute illnesses are sudden ailments that last for a short amount of time but can range in severity. For example, a headache is a form of acute illness that can be treated with over-the-counter (OTC) medicine, such as acetaminophen. On the other extreme, a heart attack is an acute illness that needs emergency medical attention and can lead to death.
What’s the difference between acute and chronic conditions? With acute conditions, patients typically experience symptoms rapidly: These symptoms are immediate and develop quickly. A cold, a broken leg, or COVID-19 are examples of acute illness. Patients with acute illnesses experience varying symptoms that progress steadily over several days to weeks. The causes of acute illnesses vary depending on the condition.
With chronic illnesses, patients typically manage their conditions, together with the physicians, over the long term. Chronic diseases, such as Crohn’s disease, heart disease, cancer, and AIDS/HIV, may be lifelong, with symptoms that worsen over time. However, they don’t always lead to fatality or a shortened life. Chronic simply refers to a condition without a cure, but often manageable. For example, diabetes and high blood pressure can be managed with prescriptions and lifestyle changes.
The following are common chronic and acute illnesses:
- Chronic illnesses:
- Diabetes describes a condition in which a patient’s body is unable to regulate the amount of sugar in the bloodstream. It’s typically caused by the lack of insulin, a hormone produced in the pancreas for blood sugar control. Diabetes can also be caused when a patient’s body is resistant to insulin.
- Coronary heart disease, also called coronary artery disease, describes when small blood vessels that supply blood and oxygen to the heart become narrowed. This narrowing can be caused by a buildup of plaque in the arteries.
- Asthma is a disease that limits the amount of air passing through the airways, causing patients to experience shortness of breath, chest tightness, and coughing. It’s caused by inflammation of the airways.
- Cancer is a disease in which abnormal or malignant cells go through uncontrolled growth in the body. The cause of many cancers is unknown, but according to MedlinePlus, it “appears to occur when the genetic material of a cell becomes changed.” Risk factors for cancer include environmental toxins, genetic problems, chemical exposure, and radiation.
- Arthritis comes in hundreds of forms. It generally describes when inflammation or degeneration occurs in one or more joints in the body.
- Acute illnesses:
- Acute bronchitis, also known as a chest cold, describes when the lungs of patients swell and produce excess mucus. It’s caused when the airways of the lungs are infected with a virus or bacterial infection.
- Influenza, or the flu, is a contagious respiratory infection that can range from mild to severe. It’s a seasonal illness caused by a virus that’s spread from person to person.
- Pneumonia describes inflammation of the alveoli, which are the air sacs of a patient’s lungs. It can be caused by bacteria, viruses, and fungi, infecting one or both lungs.
- COVID-19 is an acute respiratory condition with common symptoms that include fever, cough, and tiredness, according to the Mayo Clinic. Other symptoms include loss of taste or smell, headache, and chest pain, to name a few. The virus can spread through person-to-person transmission of respiratory droplets or contact with surfaces where the virus is present.
Healthcare managers understand these healthcare terms and implement them into systems, such as an EHR , to enable nurses and clinicians to access relevant and valid data about treatments for their patients. This helps to create efficiencies that can lead to optimized care delivery. Additionally, healthcare managers ensure that their facilities and staff have the training and resources needed to treat these illnesses. Resources can include life-saving medicine and equipment.

Anti-Inflammatory: Definition and Examples of a Key Medical Term
An understanding of anti-inflammatory medication is essential for healthcare professionals to develop strategies that consider warnings associated with anti-inflammatory medication use, side effects, and interactions with other medicines. With knowledge of anti-inflammatory medication terminology, a healthcare professional can optimize the chances of improved patient outcomes.
Non-steroidal anti-inflammatory medications (NSAIDs) are used to treat pain. Another benefit of NSAIDs is that they help control swelling and inflammation. NSAIDs work by blocking the production of enzymes called cyclooxygenase enzymes, which create a hormone-like substance that can lead to feeling pain or experiencing inflammation.
Some NSAIDs are available only with a prescription from a physician. Prescription NSAIDs are often used for musculoskeletal and orthopedic conditions, such as arthritis, tendinitis, or other inflammatory conditions. They can also be used to lower fevers and prevent blood clots. Others are available over the counter (OTC). Common OTC medications include Bayer, Advil, Motrin, and Aleve.
According to the American Academy of Family Physicians, common side effects of prescription NSAIDs may include dizziness, headache, nausea, and diarrhea. Some NSAID medications used over a longer term can increase the risk of stroke and kidney problems, according to Verywell Health. According to the Cleveland Clinic, the U.S. Food and Drug Administration requires nonaspirin NSAIDs to have warning labels about risk factors.
Common prescription NSAIDs include the following:
- Celecoxib. Celecoxib also goes by the brand name Celebrex. It relieves pain and swelling for conditions such as arthritis, acute pain, and menstrual pain.
- Fenoprofen. Fenoprofen also goes by the brand name Nalfon. It’s used to treat pain, swelling, and stiffness derived from conditions such as osteoarthritis and rheumatoid arthritis.
- Ketorolac tromethamine. Ketorolac tromethamine also goes by the brand name Toradol. It’s used to manage moderate to severe acute pain over the short term (up to five days).
- Meloxicam. Meloxicam also goes by the brand name Mobic. It’s used to reduce pain caused by osteoarthritis and rheumatoid arthritis, including juvenile rheumatoid arthritis.
- Naproxen. Naproxen also goes by the brand name Voltaren. It’s used to reduce arthritis-related pain, inflammation, and joint stiffness.
WebMd provides a list of NSAIDs available only with a prescription from a physician.
Using Standard Clinical Terminology in Care
Healthcare managers also play a pivotal role in ensuring that healthcare terms are properly used among clinical staff to protect both patients and healthcare workers. Take, for example, the use of abbreviations for healthcare terms, which enable providers to communicate information quickly and efficiently. Misinterpretation of a term may result in an incorrect dosage of a certain medicine, which can harm the patient.
Imagine a scenario in which a physician may quickly jot down on a patient’s record the abbreviation QD, which indicates that the patient should be given medication once a day. Nurses and others understand these abbreviations. However, on a hectic day, a nurse may mistakenly misinterpret the abbreviation QD as QID. This healthcare abbreviation means giving medication four times a day, instead of once a day.
This scenario shines a light on how miscommunication can harm a patient and put a healthcare facility at risk of a lawsuit. It’s the healthcare manager’s job to implement procedures that ensure that healthcare operations run optimally, which protects both patients and healthcare staff. In the example presented, a healthcare management professional could implement policies that ensure common, clear use of terms to avoid miscommunication.
This example demonstrates the danger of miscommunication in healthcare settings. The following reports offer additional insights and statistics on the consequences of miscommunication in healthcare:
- A recent study published by StatPearls reports that 7,000 to 9,000 people in the U.S. die each year due to medication errors; the misuse of abbreviations constitutes a significant cause.
- Lack of comprehension is one reason patients passively share decision-making with their physicians. This often leads to low patient satisfaction, according to a Harvard Public Health Review study. The study also notes that while low health literacy is an issue among the entire patient population, it’s “most prominent among low-income, ethnic minorities, and elderly populations.”
- Communication between healthcare providers was found to be “the root cause in more than 70% of serious medical errors,” as reported in a Safety in Health
These statistics point to the urgency of standard and clear healthcare terms, which means having a common language for effective communication between two or more people or groups in healthcare settings. Healthcare terms are essential for implementing correct healthcare procedures, delivering proper medication and treatments, and ensuring optimal and consistent patient care.
It’s also vital to ensure that patients get the information they need throughout their care. Still, according to a Brown University School of Public Health report, patients can recall only 49% of the information provided by their doctors. When healthcare terms are unclear, patients are less active in the healthcare process. Evidence, as reported by the AMA Journal of Ethics, suggests several communication barriers that hamper patients’ ability to participate in health decisions proactively. These include not knowing what a diagnosis means, a lack of understanding about their treatment options, or viewing potential health outcomes differently from their doctors. Furthermore, patients often struggle with understanding the meaning of healthcare terms such as pre-existing conditions, anti-inflammatory, and acute illness.
By ensuring the accuracy of data collected from EHRs, insurance claims systems, and other sources, healthcare managers play a pivotal role in providing a whole view of a patient. These systems, when properly integrated, inform those interacting with the patient at different points of the healthcare process on the types of care the patient has received over time. This clinical information can help determine the effectiveness of certain medicines for patients with certain conditions when added to the data of other patients. It also helps with important epidemiologic research and assessing the costs associated with care. Epidemiology is a multidisciplinary, scientific method of identifying what causes diseases, where they originate, and methods to control their spread. This information is critical to public health.
Standardization of clinical terminology is also essential for ensuring that the data is useful throughout the healthcare infrastructure. The common use of clinical terminology enables the interoperability of clinical and patient data systems, which means that the data on one system means the same thing on another. This sharing of clinical terminology across different systems is central to informatics: “the science of how to use data, information, and knowledge to improve human health and the delivery of health care services,” according to the American Medical Informatics Association.
Healthcare managers play an important role in the use of standard clinical terminology in healthcare, which significantly benefits patients at the point of care by improving diagnostic and treatment outcomes. Standard clinical terminology enables the transparent exchange of information that minimizes the chance of ambiguity, misinterpretation, and life-threatening mistakes.
Additional information about clinical terminology
- “Standards in Healthcare Data” examines how data standards, quality, and implementation can improve clinical data interoperability and drive continuous improvement.
- “Terminology Services: Standard Terminologies to Control Health Vocabulary” describes the usefulness of a terminology server to facilitate the management of health information and improve system interoperability.
- The Healthcare Information and Management Systems Society describes common terminology standards in health information and technology. It explains that they’re essential for ensuring the effectiveness of information exchange and interoperability.
- Articles from Forbes and WebMD inform readers on the basics of insurance policy, explicitly describing key insurance and healthcare terms, such as coinsurance, out-of-pocket maximum, COBRA, and flexible spending accounts.
- The “Glossary of Health Coverage and Medical Terms” from the U.S. Department of Labor is a handy resource that provides definitions of commonly used healthcare terms.
Additional Sources
Centers for Disease Control and Prevention, Antibiotic Prescribing and Use in Doctor’s Offices
Deloitte, “Inside the Patient Journey: Three Key Touch Points for Consumer Engagement Strategies”
Healthline, “Everything You Need to Know About Pneumonia”
National Library of Medicine, UMLS Learning Resources
Verywell Health, “The Difference Between Acute and Chronic Illnesses”
Wolters Kluwer, “How to Use Standardized Healthcare Terminologies to Meet Your Quality Care Goals”

